Occupational therapy brings normal life back to many hurting people, and a pediatric occupational therapy assistant has a special place working with children. If you aren’t afraid to dive in and help people ease back into their daily routines, and you enjoy working with kids, you might fit right into the pediatric OTA world.
Job security, growth, and opportunity
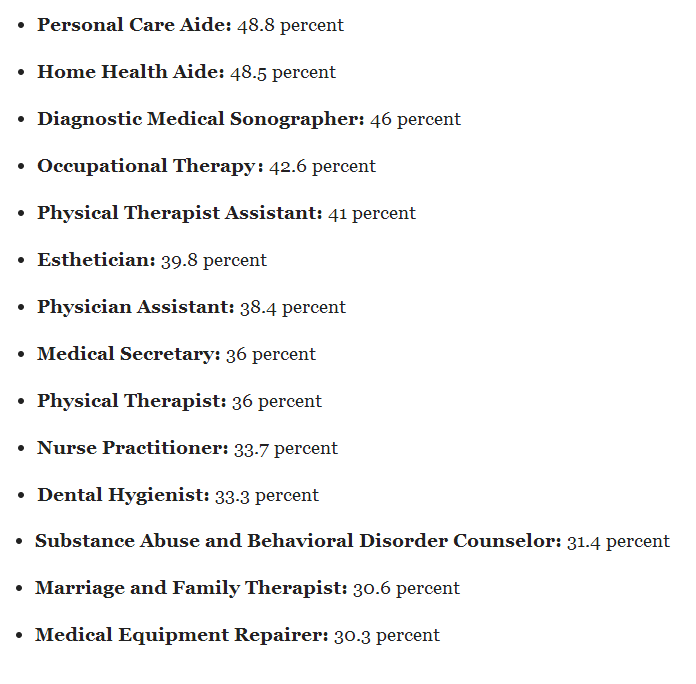
There aren’t many career paths that offer above-average wages in an industry growing six times faster than the national average. When you’re a pediatric occupational therapy assistant, you’re in a field that’s always hiring — and it requires only five semesters of school. The average salary for an OTA is $54,520 per year, or $26.21 per hour, and the field is expected to grow by 40 percent between 2014 and 2024. Now that’s some growth we can get behind!
What is a pediatric OTA, and how is it different from other OTA specialties?
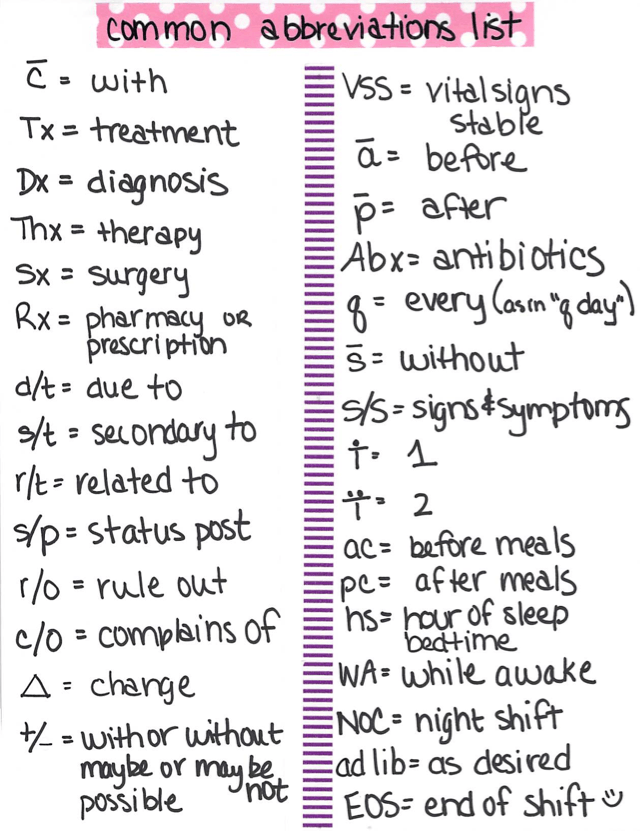
Occupational therapy assistants help people who have physical, sensory, or cognitive disabilities. OTAs help people learn the everyday skills they need in order to live and enjoy life as independently as possible, like getting dressed or brushing teeth. OTA care happens in the home, community clinics, rehab facilities, schools, or physicians’ offices.
Occupational therapists identify issues and create a care plan for a patient’s needs, and OTAs execute that plan. Therapy may include helping patients with therapeutic activities like stretches and other exercises, leading activities that promote coordination and socialization, encouraging completion of activities and tasks, and administrative duties.
Pediatric OTAs do the same thing for children. Kids may have physical or cognitive needs, or they may be recovering from an injury. An OTA helps while a child is recovering from injury or illness at home and in the classroom. A friendly smile and playful approach go a long way toward comforting a scared child who may be in pain, and perhaps self-conscious about not being as independent as they want.
Common conditions that require an OTA
Everyone has a job, and a child’s job is to play, learn, and socialize. When kids struggle with these tasks, a pediatric occupational therapist and their assistant work with the child and their family to help them succeed in daily activities.
Kids who need an OTA may have congenital issues, such as cerebral palsy, muscular dystrophy, spina bifida, autism, or mental or emotional health problems. These young patients may also be dealing with injury from a traumatic event, such as a missing limb or amputation, head injuries, severe burns, or spinal cord trauma.
Pediatric occupational therapy assistants have an opportunity to make a positive difference in young lives who could use a helping hand and a smile. If you’re considering a new career in healthcare, you love kids, and you don’t want to spend years in school, consider becoming a pediatric OTA.