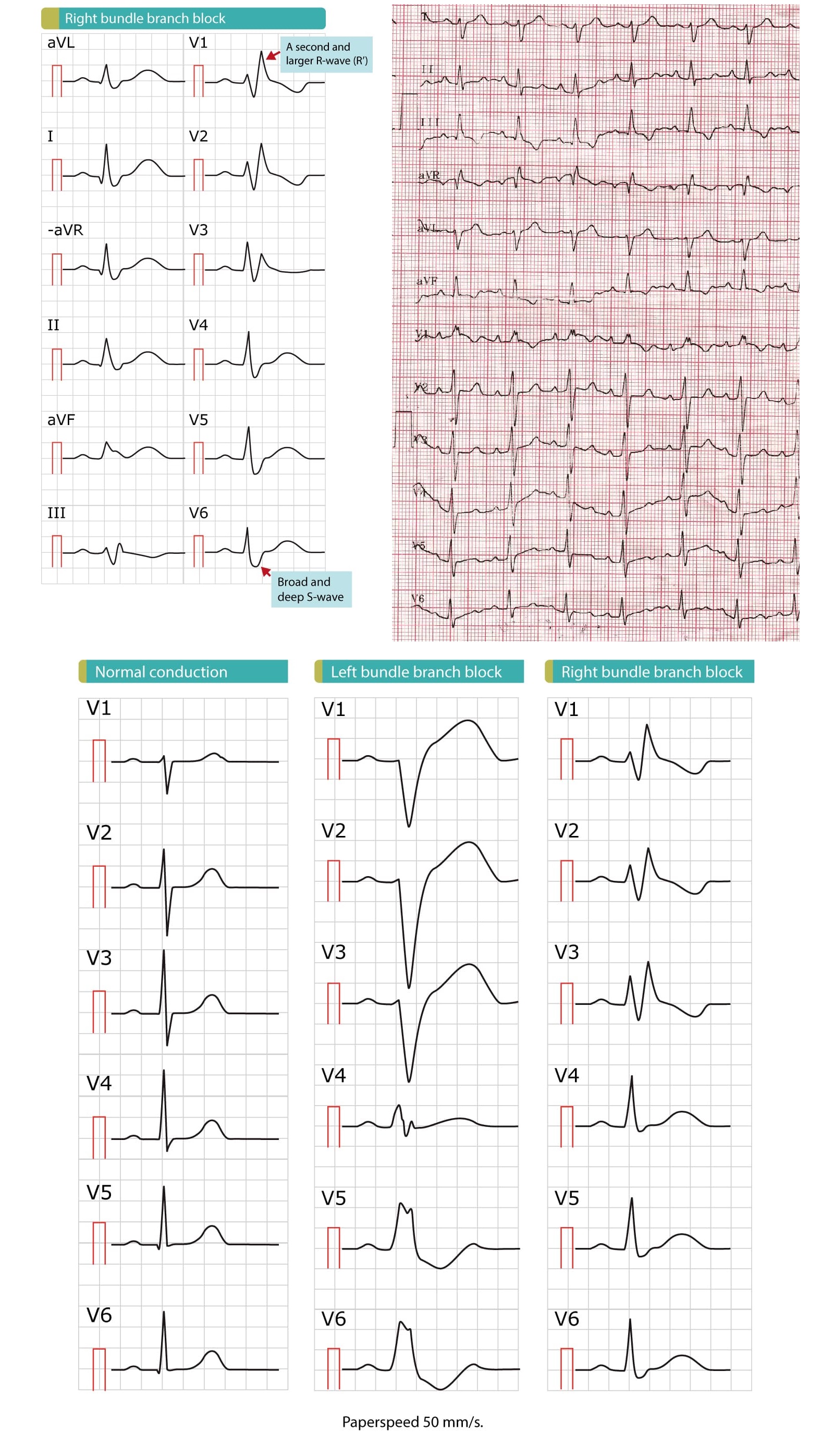
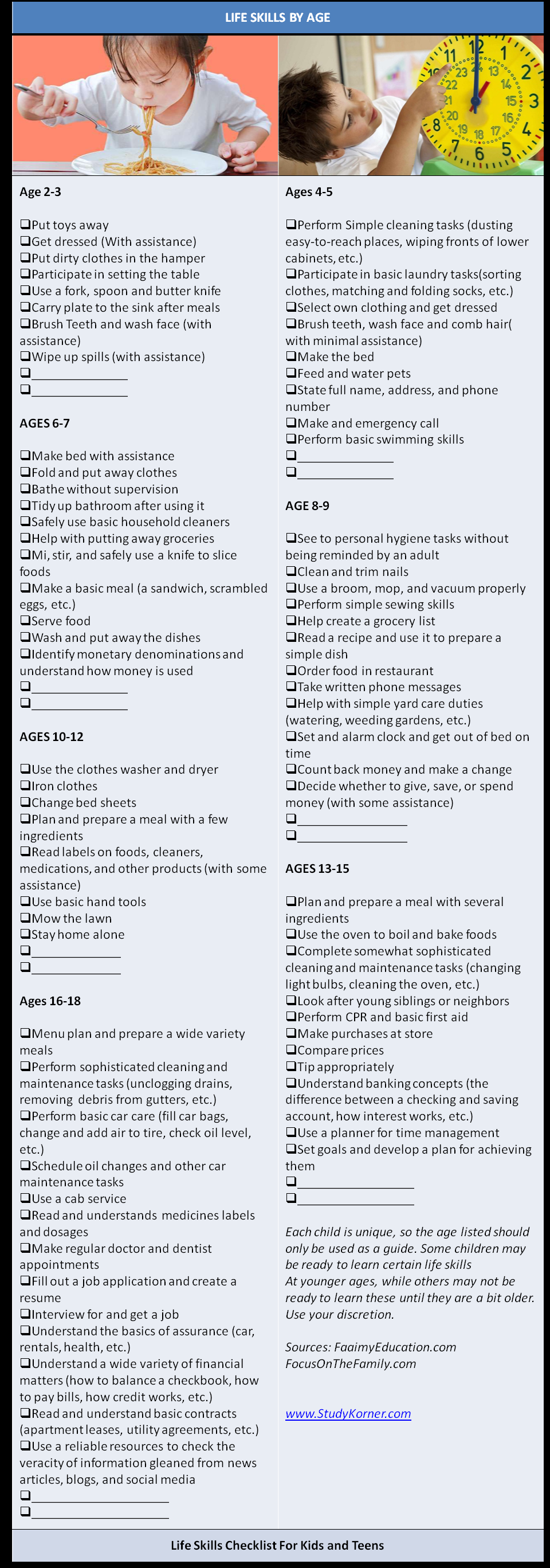
The ECG criteria for a right bundle branch block include the following: QRS duration greater than 120 milliseconds. rsR’ “bunny ear” pattern in the anterior precordial leads (leads V1-V3) Slurred S waves in leads I, aVL and frequently V5 and V6.
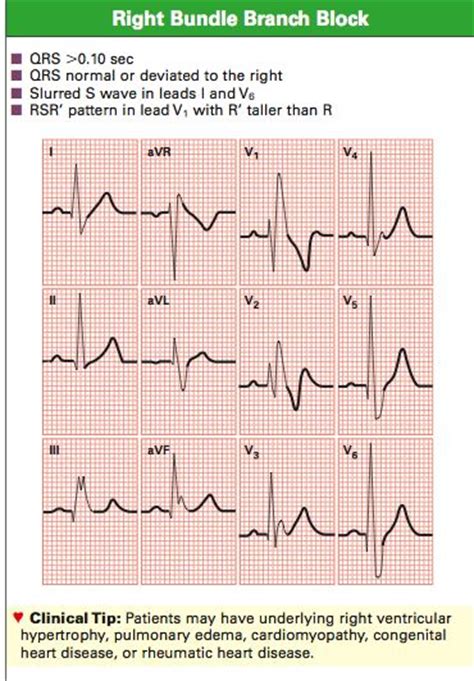
The ECG criteria for diagnosing right bundle branch block (RBBB) typically include the following:
QRS duration greater than 120 milliseconds: The QRS complex, which represents ventricular depolarization, is wider than normal due to delayed activation of the right ventricle.
rsR’ “bunny ear” pattern in the anterior precordial leads (leads V1-V3): The QRS complex shows an initial small r wave, followed by a larger R wave, and a second smaller r’ wave that gives the appearance of bunny ears.
Slurred S waves in leads I, aVL and frequently V5 and V6: The S wave, which represents initial negative deflection in the QRS complex, is prolonged and has a slurred appearance in the lateral leads I, aVL, and V5-V6.